Type 2 diabetes happens when the body
cannot use insulin correctly and sugar builds up in the blood. It was once
called adult-onset diabetes.
Over time, high blood sugar levels in
type 2 diabetes can damage the eyes, kidneys, nerves and heart. This can happen
because the pancreas doesn't make enough of a hormone called insulin that helps
sugar enter the cells. It is also because the cells respond poorly to insulin
by taking in less sugar.
Both type 1 and type 2 diabetes can begin
during childhood and adulthood. Type 2 is more common in older adults. But the
increase in the number of children with obesity has led to more young people
with type 2 diabetes.
There's no cure for type 2 diabetes.
Losing weight, eating well and exercising can help manage the condition. If
diet and exercise aren't enough to manage blood sugar, diabetes medicines or
insulin therapy may help.
SYMPTOMS
Symptoms of type 2 diabetes often come on slowly. In fact, people can
live with type 2 diabetes for years and not know it. When there are symptoms,
they may include:
More thirst.
More
urination.
More hunger.
Weight loss.
Tiredness.
Blurred
vision.
Slow-healing
sores.
Frequent
infections.
Numbness or
tingling in the hands or feet.
Areas of
darkened skin, most often in the armpits and neck.
Causes
Type 2 diabetes is mainly the result of two issues:
Cells in
muscle, fat and the liver don't respond to insulin as they should. As a result,
the cells don't take in enough sugar.
The gland that
makes insulin, called the pancreas, can't make enough to keep blood sugar
levels within a healthy range.
Being overweight and not moving enough are key factors.
How insulin works
Insulin is a hormone that comes from a gland. The gland is called the
pancreas. Insulin manages how the body uses sugar in the following ways:
Sugar in the
bloodstream causes the pancreas to release insulin.
Insulin in the
bloodstream gets sugar into the cells.
The amount of
sugar in the bloodstream drops.
Then the
pancreas releases less insulin.
The role of glucose
A sugar called glucose is a main source of energy for the cells that
make up muscles and other tissues.
Glucose comes
from two major sources. They are food and the liver.
Glucose goes
into the bloodstream. There it enters cells with the help of insulin.
The liver
stores glucose in the form of glycogen and also makes glucose.
When glucose
levels are low, the liver breaks down stored glycogen into glucose. This keeps
the body's glucose level within a healthy range.
In type 2 diabetes, this process doesn't work well. Instead of moving
into the cells, sugar builds up in the blood. As blood sugar levels rise, the
pancreas releases more insulin. Over time, the cells in the pancreas that make
insulin are damaged. Then the cells can't make enough insulin to meet the
body's needs.
Risk factors
Factors that may increase the risk of type 2 diabetes include:
Excess weight. Being overweight or obese is a main risk.
Waist size. Storing fat mainly in the belly rather than
in the hips and thighs raises the risk. The risk of type 2 diabetes is higher
in people assigned male at birth whose waists measure more than 40 inches
(101.6 centimeters). For people assigned female at birth, a waist measure of
more than 35 inches (88.9 centimeters) raises the risk.
Sitting. The less active a person is, the higher the
risk. Physical activity helps manage weight, uses up glucose as energy and
helps cells take in insulin.
Family history. Having a parent or
sibling who has type 2 diabetes raises the risk.
Race and ethnicity. It's not clear why,
but people of certain races and ethnicities are more likely to get type 2
diabetes than white people are. Races and ethnicities include Black people,
Hispanic people, Native American and Asian people, and Pacific Island people.
Blood lipid levels. A higher risk is
linked with low levels of high-density lipoprotein. Also called HDL
cholesterol, this is the "good" cholesterol. Higher risk also is
linked with high levels of a certain type of fat in the blood, called
triglycerides.
Age. The risk of type 2 diabetes goes up with age,
mainly after age 35.
Prediabetes. Prediabetes is a condition in which blood
sugar is higher than the standard range, but not high enough to be called type
2 diabetes. If not treated, prediabetes often moves on to become type 2
diabetes.
Pregnancy-related risks. The risk
of getting type 2 diabetes is higher in people who had gestational diabetes
when they were pregnant. And it's higher in those who gave birth to a baby
weighing more than 9 pounds (4 kilograms).
Polycystic ovary syndrome. This
condition results in irregular menstrual periods, excess hair growth and
obesity. It raises the risk of diabetes.
Complications
Type 2 diabetes affects many major organs. These include the heart,
blood vessels, nerves, eyes and kidneys. Also, factors that raise the risk of
diabetes are risk factors for other serious diseases.
Heart and blood vessel disease. Diabetes
is linked with a higher risk of heart disease, stroke, high blood pressure and
narrowed blood vessels, called atherosclerosis.
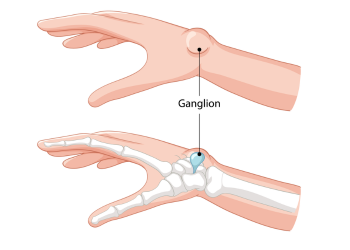
Nerve damage in arms and legs. This
condition is called neuropathy. High blood sugar over time can damage or
destroy nerves. Neuropathy may cause tingling, numbness, burning, pain or loss
of feeling. It most often begins at the tips of the toes or fingers and slowly
spreads upward.
Other nerve damage. Damage to nerves of
the heart can cause irregular heart rhythms. Nerve damage in the digestive
system can cause problems with nausea, vomiting, diarrhea or constipation.
Nerve damage also may cause erectile dysfunction.
Kidney disease. Diabetes may lead to
long-term kidney disease or end-stage kidney disease that can't be reversed.
End-stage kidney disease may need to be treated with mechanical filtering of
the kidneys, called dialysis, or a kidney transplant.
Eye damage. Diabetes increases the risk of serious eye
conditions. Conditions include cataracts and glaucoma. Diabetes also may damage
the blood vessels of the retina, which is the part of the eye that senses
light. This is called diabetic retinopathy. This damage can lead to blindness.
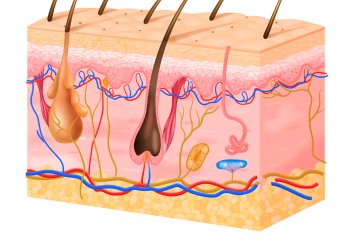
Skin conditions. Diabetes may raise
the risk of some skin problems. Skin problems may include bacterial and fungal
infections.
Slow healing. Cuts and blisters that aren't treated can
become serious infections. The infections may heal poorly.
Hearing impairment. Hearing problems are
more common in people with diabetes.
Sleep apnea. Obstructive sleep apnea is common in people
who have type 2 diabetes. Obesity may be the main cause of both conditions.
Dementia. Type 2 diabetes seems to raise the risk of
Alzheimer's disease and other conditions that cause dementia.
Prevention
Healthy lifestyle choices can help prevent type 2 diabetes. If you have
prediabetes,lifestyle changes may slow the condition or keep it from becoming
diabetes.
A healthy lifestyle includes the following:
Eat healthy foods. Choose foods lower
in fat and calories and higher in fiber. Focus on fruits, vegetables and whole
grains.
Be active. Aim for 150 or more minutes a week of
moderate to vigorous aerobic activity, such as brisk walking, bicycling,
running or swimming.
Lose weight. If you are overweight, losing some weight and
keeping it off may slow prediabetes from becoming type 2 diabetes. If you have
prediabetes, losing 7% to 10% of your body weight may lower the risk of
diabetes.
Don't sit for long. Sitting for long
periods can raise the risk of type 2 diabetes. Get up every 30 minutes and move
around for at least a few minutes.
Diagnosis
The glycated hemoglobin test most often diagnoses type 2 diabetes. Also
called the A1C test, it reflects the average blood sugar level for the past two
to three months. Results mean the following:
Below 5.7% is
healthy.
5.7% to 6.4%
is prediabetes.
6.5% or higher
on two separate tests means diabetes.
If there are no A1C tests or if you have certain conditions that get in
the way of A1C test results, your healthcare professional may use the following
tests to diagnose diabetes:
Random blood sugar test. Blood sugar values show in milligrams of sugar per deciliter
(mg/dL) or millimoles of sugar per liter (mmol/L) of blood. It doesn't matter
when you last ate. A level of 200 mg/dL (11.1 mmol/L) or higher suggests
diabetes. This is most likely if you also have symptoms of diabetes, such as
urinating often and being very thirsty.
Fasting blood sugar test. You give a blood sample for testing after not eating overnight.
Results are as follows:
Less than 100
mg/dL (5.6 mmol/L) is healthy.
100 to 125
mg/dL (5.6 to 6.9 mmol/L) is prediabetes.
126 mg/dL (7
mmol/L) or higher on two tests is diabetes.
Oral glucose tolerance test. This mainly tests the blood sugar of people who are pregnant and
those who have cystic fibrosis. You don't eat for a certain amount of time.
Then you drink a sugary liquid at your healthcare team's office. You give blood
samples over two hours to test blood sugar levels. Results are as follows:
Less than 140
mg/dL (7.8 mmol/L) after two hours is healthy.
140 to 199
mg/dL (7.8 mmol/L and 11.0 mmol/L) is prediabetes.
200 mg/dL
(11.1 mmol/L) or higher after two hours suggests diabetes.
Screening
People younger
than 35 who are overweight or obese and have one or more risk factors linked to
diabetes.
Women who had
diabetes while pregnant, called gestational diabetes.
People who
have been diagnosed with prediabetes.
Children who
are overweight or obese and who have a family history of type 2 diabetes or
other risk factors.
Treatment
Living with type 2 diabetes involves learning about the condition and
lifestyle changes. Diabetes education is an important part of managing the
condition. Management includes:
Healthy
eating.
Regular
exercise.
Weight loss if
needed.
Diabetes
medicine or insulin therapy if needed.
Keeping track
of blood sugar.
These steps make it more likely that blood sugar will stay in a healthy
range. And they may help delay or prevent complications.
Healthy eating
There's no diabetes diet. But it's good to focus your eating on:
A regular
schedule for meals and healthy snacks.
Smaller
amounts of food.
More
high-fiber foods, such as fruits, nonstarchy vegetables and whole grains.
Fewer refined
grains, starchy vegetables and sweets.
Modest
servings of low-fat dairy, low-fat meats and fish.
Healthy
cooking oils, such as olive oil or canola oil.