Metabolic dysfunction-associated steatotic liver disease (MASLD),
formerly called nonalcoholic fatty liver disease (NAFLD), is a liver condition
that affects people with excess weight, obesity or other metabolic conditions,
such as type 2 diabetes, high blood pressure or high cholesterol. In MASLD, too
much fat builds up in the liver.
MASLD is becoming more common, especially in Middle Eastern and Western
nations, as the number of people with obesity rises. It is the most common form
of liver disease in the world. MASLD ranges in severity from hepatic steatosis
— sometimes called diffuse hepatic steatosis, or formerly fatty liver
infiltration or simply fatty liver — to a more severe form of disease called
metabolic dysfunction-associated steatohepatitis (MASH), formerly called
nonalcoholic steatohepatitis (NASH).
MASH causes the liver to swell or enlarge. This is known as hepatomegaly.MASH also causes fat deposits in the liver, which causes liver damage.
MASH may get worse and may lead to serious liver scarring, called cirrhosis,or evenliver cancer.
Symptoms
Not feeling
well, known as malaise.
Pain or
discomfort in the upper right belly area.
Possible symptoms of MASH and cirrhosis, which is severe scarring,
include:
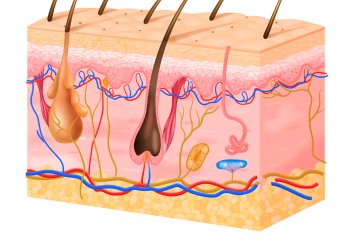
Itchy skin.
Abdominal
swelling, also called ascites
Shortness of
breath.
Swelling in
the legs.
Spiderlike
blood vessels just beneath the skin's surface.
Enlarged
spleen.
A change in
skin color on the palms.
Yellowing of
the skin and eyes
Causes
Genetics.
Being
overweight or having obesity.
Insulin resistance,which happens when the body's cells don't take up sugar in response to
the hormone insulin.
Type 2
diabetes, sometimes called high blood sugar or hyperglycemia.
High levels of
fats, especially triglycerides, in the blood.
These combined health concerns may contribute to liver damage. However,
some people get MASLD even if they do not have any risk factors.
Risk factors
Obesity, especially when fat is
centered in the waist.
Type 2 diabetes.
High cholesterol.
High levels of triglycerides in the
blood.
Insulin resistance.
Polycystic ovary syndrome.
Obstructive sleep apnea.
Underactive thyroid, also called
hypothyroidism.
Underactive pituitary gland, also called hypopituitarism.
Growth hormone deficiency
MASH is more likely in people:
Older than 50.
certain genetic risk factors.
With obesity.
With diabetes or high blood sugar.
With symptoms of metabolic
syndrome, such as high blood pressure ,high triglycerides and a large waist size.
Severe liver scarring, also called cirrhosis, is the main complication
of MASLD and MASH. Cirrhosis happens because of liver injury, such as the
damage caused by inflammation in MASH. As the liver tries to stop inflammation,
it creates areas of scarring, also called fibrosis.
If nothing is done to stop the scarring, cirrhosis can lead to:
Fluid buildup
in the stomach area, called ascites.
Swollen veins
in the esophagus, called esophageal varices, which can rupture and bleed.
Confusion,
sleepiness and slurred speech, also called hepatic encephalopathy.
Overactive
spleen, known as hypersplenism, which can cause too few blood platelets.
Liver cancer.
End-stage
liver failure, which means the liver has stopped working.
For many people with MASLD, the outlook is good, especially if they make
recommended lifestyle changes. In fact, in some people, weight loss may help
reverse MASLD.
Prevention
Eat a healthy diet. Eat a diet that's rich in fruits, vegetables,
whole grains and healthy fats. One such diet is the Mediterranean diet.
Limit alcohol, simple sugars and portion sizes. Avoid sugary drinks such as soda, sports drinks, juices and sweet
tea. Avoid or limit alcohol, which can damage the liver.
Keep a healthy weight. If you
are overweight or have obesity, work with your healthcare team to gradually
lose weight. If you are at a healthy weight, work to keep it by eating a
healthy diet and exercising.
Exercise. Be active most days of the week.
Diagnosis and tests
Blood tests
Liver enzyme
and liver function tests.
Complete blood count.
Iron studies,
which show how much iron is in the blood and other cells.
Tests for
chronic viral hepatitis, which includes hepatitis B and hepatitis C.
Celiac disease
screening test.
Measurement of
fasting blood sugar.
A1C testwhich shows how stable your blood sugar is.
Lipid profilewhich measures blood fats such as cholesterol and triglycerides.
Abdominal ultrasoundwhich is often the first
test used when liver disease is suspected.
Magnetic resonance imaging (MRI) or computerized tomography (CT)
scanningThese tests are better at finding excess liver
fat and cirrhosis.
Transient elastographya newer type
of ultrasound that measures the stiffness of the liver. Liver stiffness is a
sign of scarring, also called.
Magnetic resonance elastography which combines MRI with sound waves to create
a visual map, also called an elastogram, showing the stiffness of body tissues.
Liver Biopsy